Conformity Assessment Guide: EU MDR and IVDR Compliance Strategies
Achieving compliance with regulatory requirements is a critical aspect for manufacturers of medical devices and in vitro diagnostic devices (IVDs) seeking market access within the European Union. The EU Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR) have introduced a comprehensive framework for conformity assessments, which are examinations of a manufacturer’s technical documentation and quality management system.
Comprehending Different Conformity Routes: A Necessity
Navigating the conformity assessment process requires a thorough understanding of the different routes and options available for various risk classifications of medical devices and IVDs. Failure to grasp the intricacies of these routes can lead to significant delays, increased costs, and potential market access hurdles. By comprehending the distinct requirements and annexes associated with each risk classification, manufacturers can make informed decisions and streamline their compliance process.
Conformity Assessment Routes and Options Explained
The EU MDR and IVDR have established specific routes and options for conformity assessments based on the risk classification of medical devices and IVDs. Understanding these classifications is crucial for manufacturers to determine the appropriate pathway to demonstrate compliance.
Each conformity assessment route is governed by specific annexes within the regulations, which outline the technical documentation and QMS requirements. Manufacturers must adhere to the relevant applicable annexes (i.e., Annex IX, X, XI for both MDR and IVDR) when preparing their submissions. Comprehensive technical files, risk management documentation, and robust quality management systems are essential for demonstrating compliance.
Routes of Conformity Under the EU MDR
- Class I Devices
- Low-risk devices: Self-certification by the manufacturer
- Sterile, measuring, or reusable surgical instruments: Limited notified body involvement
- Class IIa Devices (Medium Risk)
- Option 1: Quality Management System (QMS) certification (e.g., ISO 13485) and technical documentation assessment
- Option 2: Technical documentation review (representative device) and production quality assurance
- Class IIb Devices (Medium Risk)
- QMS certification and technical documentation assessment (representative device per generic group)
- Class IIb Implantable Devices (Higher Risk)
- Option 1: QMS certification, technical documentation assessment (excluding certain dental implants)
- Option 2: Type examination (product design review), QMS assessment, and production quality assurance
- Class III Devices (Higher Risk)
- Option 1: QMS certification and technical documentation assessment
- Option 2: Type examination, QMS assessment, and production quality assurance
Routes of Conformity Under the EU IVDR
- Class A Devices (Low Risk)
- Self-certification for non-sterile devices
- Limited notified body involvement for sterile devices
- Class B Devices (Medium Risk)
- Self-testing and near-patient testing: QMS certification, technical documentation (sections 4.4-4.8)
- Other devices: QMS certification, technical documentation (sections 4.4-4.8, 5.1)
- Class C Devices (Higher Risk)
- Option 1: QMS certification, technical documentation (sections 4.4-4.8, 5.1, 5.2) for each device
- Option 2: Not applicable for companion diagnostics
- Class D Devices (Higher Risk)
- Option 1: QMS certification, technical documentation (excluding sections 5 and 6, or including all chapters for companion diagnostics)
- Option 2: Type examination, QMS assessment, production quality assurance
The Conformity Assessment Process
Understanding the steps involved in the conformity assessment process helps manufacturers prepare effectively and manage expectations. This section outlines the key stages of the process and highlights the role of notified bodies.
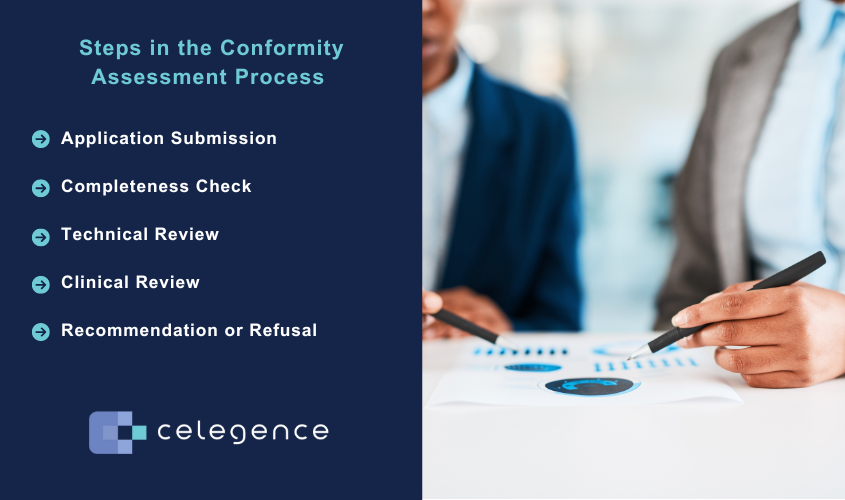
Steps in the Conformity Assessment Process
- Application Submission
- Manufacturers submit their initial application to a chosen notified body
- Application includes relevant technical documentation and quality management system information
- Completeness Check
- Notified body reviews the submitted documents for completeness
- Ensures all required sections and elements are present • Not an in-depth review of data, but a verification of document availability
- Technical Review
- Detailed examination of technical documentation
- Assessment of compliance with relevant standards and regulations
- Review of test results, risk management, and product specifications
- Clinical Review
- Evaluation of clinical evidence and performance data
- Assessment of post-market surveillance plans
- Review of clinical evaluation reports and benefit-risk analyses
- Recommendation or Refusal
- Notified body makes a decision based on the assessment results
- Recommendation for CE marking if requirements are met
- Refusal if significant non-conformities are identified
Note:
- Multiple rounds of questions may occur during technical and clinical reviews.
- Limited to three rounds in most cases.
- Possibility of requesting extensions for complex issues (up to 90 days total).
- Potential for immediate refusal if gaps are deemed insurmountable after initial review.
Role of Notified Bodies
- Act as independent third-party assessors.
- Evaluate manufacturer compliance with regulatory requirements.
- Raise questions during the review process.
- The Notified Bodies will not offer regulatory consultation.
Common Pitfalls and Challenges
- Incomplete Technical Files
- Insufficient data to support claims
- Inadequate risk management documentation
- Cost Considerations
- High notified body fees
- Additional costs for addressing non-conformities
- Tight Timelines for Responses
- 30-day standard response window for clarifications
- Difficulty gathering necessary data quickly
- Lack of Detail for Clinical Reviewers
- Insufficient explanation of clinical rationale
- Inadequate summaries of investigations
- Limited benefit-risk discussions
Best Practices for Conducting a Conformity Assessment Process
Effective Conformity Assessment Project Management
- Start early: Begin preparations well in advance of the submission and any communicated deadlines.
- Create a detailed project plan: Outline all required tasks and allocate resources accordingly.
- Set realistic timelines: Account for potential delays and revision cycles.
- Monitor progress regularly: Track milestones and adjust plans as needed.
- Allocate sufficient resources: Ensure dedicated personnel are available throughout the process.
Key Effective Practices of the Manufacturer
- Establish a single point of contact: Designate a team member to manage all interactions.
- Respond promptly: Address queries and requests within specified timeframes (typically within 30 days).
- Be proactive: Inform notified bodies of any anticipated delays or challenges.
- Seek clarification: Ask questions when instructions or requirements are unclear.
- Document all interactions: Maintain a record of communications for future reference.
- Transparency regarding any challenges or delays in addressing non-conformities.
- Clear and concise communication from manufacturers.
Well-Organized Technical Documentation
- Follow regulatory guidelines: Adhere to the structure outlined in key MDCG and notified body issued guidelines for a streamlined process.
- Use clear headings and subheadings: Organize information logically and consistently.
- Include a comprehensive table of contents: Enable easy navigation through the document.
- Employ bookmarks in PDF files: Facilitate quick access to specific sections.
- Utilize visual aids: Incorporate diagrams, tables, and images to enhance clarity.
- Ensure consistency: Use uniform terminology and formatting throughout.
For a successful conformity assessment, plan early, manage timelines effectively, and allocate resources wisely. Maintain clear communication, respond promptly, and document all interactions. Ensure your documentation is well-organized and includes comprehensive clinical analysis while addressing any clinical data gaps.
Successful Conformity Assessment: Key Takeaways
Achieving EU MDR and IVDR compliance is vital for medical device and IVD manufacturers seeking market access in the European Union. By understanding different conformity assessment routes and requirements, manufacturers can avoid delays and ensure regulatory adherence. Preparing thorough technical documentation, maintaining clear communication with notified bodies, and addressing common challenges can streamline the process.
Effective planning, good quality clinical data, and following regulatory guidelines contribute to a successful outcome. With a proactive approach and strategic preparation, manufacturers can enhance their success rates of achieving market access.
About Celegence
Celegence, led by Sonia Veluchamy is more than a regulatory consulting firm. We are a strategic partner specializing in EU MDR and IVDR requirements, ensuring they are efficient, accurate, and compliant.
Celegence is here to help with our expert solutions and advanced AI technology. Contact us or reach out to us at info@celegence.com to learn more about how Celegence could be your partner.
About The Author

This blog is authored by Joseph Richardson Larbi, MSc. RA. He’s the Director of Medical Device Regulatory Affairs at Celegence with over 20 years of expertise in life cycle management and quality systems. His experience spans diabetes management devices, nicotine replacement therapy, and more, having worked with renowned companies like Roche and OBG Pharmaceuticals


